Welcome to the Farncombe Family Digestive Health Research Institute
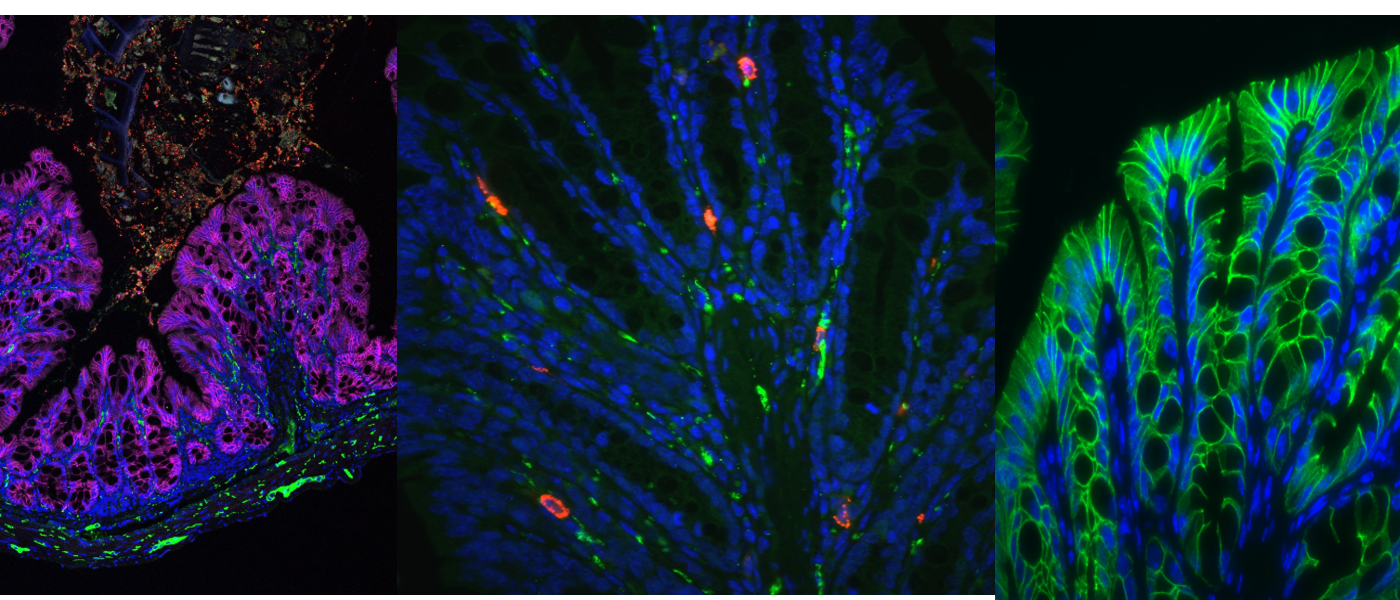
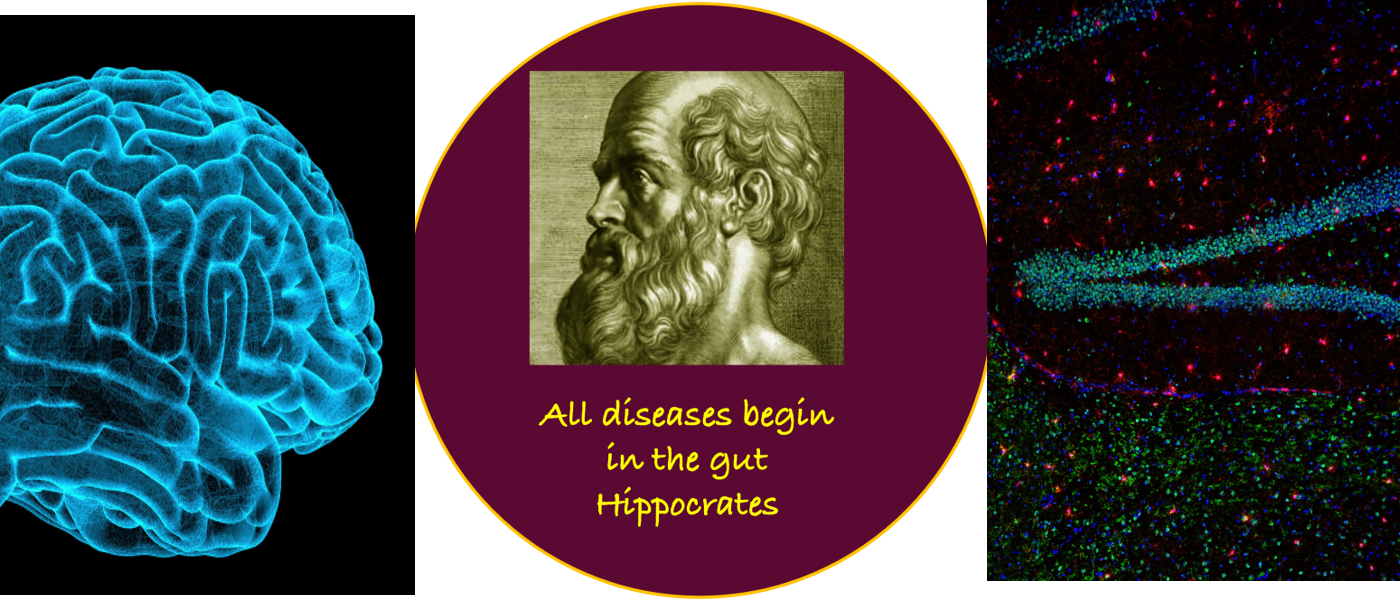
The Farncombe Family Digestive Health Research Institute was established in 2008, replacing McMaster University’s Intestinal Disease Research Program that had been in existence since 1984. The Institute’s goal is to better understand and treat, and ultimately cure, the most common categories of chronic illness within and beyond the gut, including the brain and with a focus on the intestinal microbiota. The Institute pursues its vision by adopting an integrated multidisciplinary approach that encompasses bench-to-bedside research and involves close collaborations between clinicians, clinician-scientists and basic scientists. The vision also mandates the provision of the best possible experience that will enable our trainees to pursue successful careers in the academic and private sectors. Knowledge evaluation and translation is a key aspect of our vision, serving to inform peers and the public of advances in our understanding of digestive diseases, and to increase awareness of the burden of these diseases on our society.